Ankylosing Spondylitis (AS): Chronic Inflammatory Spine Disease
Ankylosing Spondylitis
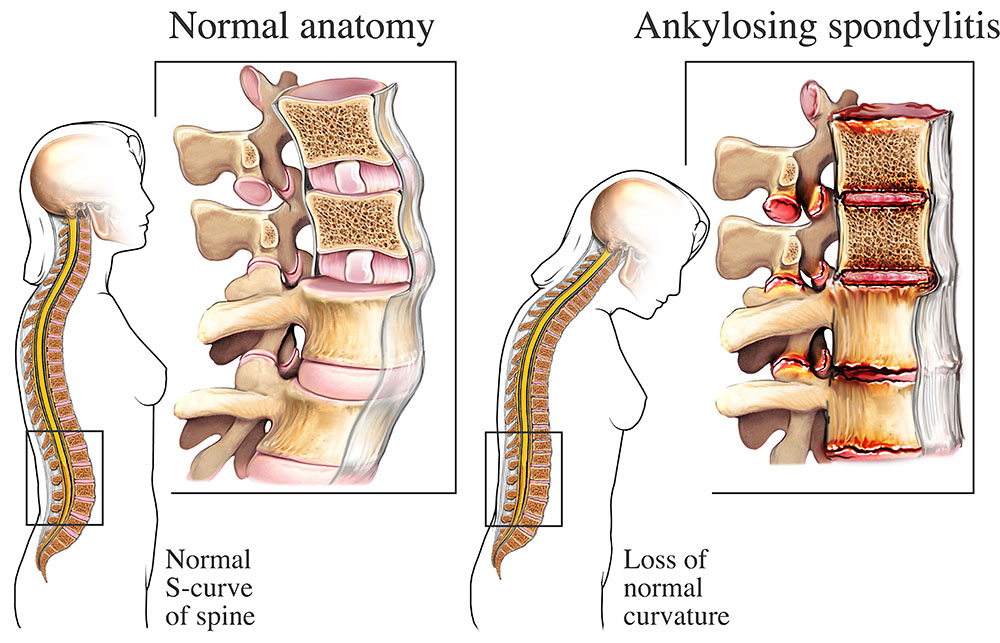
Ankylosing Spondylitis is a long-term inflammatory condition primarily affecting the spine and sacroiliac joints, leading to pain, stiffness, and reduced mobility.
❓ What is Ankylosing Spondylitis?
Ankylosing Spondylitis (AS) is a chronic form of inflammatory arthritis that primarily impacts the spine, although other joints can also be involved. The condition causes inflammation at the junctions where ligaments and tendons attach to bones, particularly in the spine and pelvis. This can result in persistent back pain and stiffness. Over time, chronic inflammation may cause the vertebrae to fuse, leading to decreased spinal flexibility and, in advanced cases, a forward-stooped posture.
⚠️ Symptoms of Ankylosing Spondylitis
-
Ongoing lower back and hip stiffness, especially after rest or in the morning
-
Fatigue and discomfort in the neck or spine
-
Gradual spread of pain and stiffness upward along the spine
-
In advanced stages, chest expansion may be limited, affecting breathing
🧬 What Causes Ankylosing Spondylitis?
The precise cause of AS is unknown, but there is a strong genetic component. The HLA-B27 gene is found in most individuals with AS, although having the gene does not guarantee development of the disease. Environmental factors may also contribute to disease onset in genetically susceptible individuals.
🔍 Risk Factors for Developing AS
-
Age: Usually begins between the ages of 17 and 35
-
Gender: More frequently diagnosed in males
-
Family History: A close relative with AS increases your likelihood
-
Genetics: Presence of HLA-B27 is a known genetic marker
🩺 How is AS Diagnosed?
-
Clinical Exam: Evaluating spinal mobility, pain areas, and posture
-
Laboratory Testing: Identifying inflammatory markers and testing for HLA-B27
-
Imaging: X-rays and MRI scans can reveal inflammation or fusion in the sacroiliac joints and spine
👨⚕️ Who Manages AS?
Diagnosis and management should be handled by a rheumatologist, a specialist in autoimmune and joint diseases. In complex cases, care may involve collaboration with physical therapists, ophthalmologists (for eye symptoms), or pulmonologists.
💊 Treatment Approaches for AS
-
Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), tumor necrosis factor (TNF) blockers, and other biologic therapies
-
Physical Therapy: Essential for maintaining mobility and posture
-
Exercise: Daily activity improves spinal flexibility and overall function
⚠️ Potential Complications of AS
-
Spinal Fusion: Can severely reduce mobility and cause deformity
-
Chronic Pain: Persistent inflammation may limit daily activities
-
Uveitis: An eye condition causing redness, pain, and visual disturbances
-
Lung Function Impairment: Resulting from reduced rib cage movement
🧘♀️ Self-Care Tips for Living with AS
-
Perform regular stretching exercises to support flexibility
-
Focus on good posture habits throughout the day
-
Avoid smoking, which can worsen lung and spinal health
-
Maintain an active lifestyle to support joint health and mood
